Exercising and Managing Breathlessness with Chronic Lung Conditions
Living with a chronic respiratory condition such as asthma, COPD, bronchiectasis, or interstitial lung disease can make physical activity feel overwhelming. Many people with breathing difficulties avoid exercise due to fear of breathlessness or worsening symptoms. However, staying active is essential for maintaining lung function, overall health, and quality of life.
The key is to exercise safely, manage symptoms effectively, and use strategies that help control breathlessness. Whether you have asthma, COPD, or another chronic lung condition, this guide will help you stay active while protecting your respiratory health.
Why Exercise is Important for People with Chronic Respiratory Conditions
While breathlessness during exercise can be uncomfortable, avoiding physical activity can lead to:
If you are struggling with unexplained weight gain, difficulty losing weight, or disrupted sleep, it may be time to explore the relationship between sleep disorders and weight gain.
- Weakened respiratory muscle strengths, makes performing daily tasks harder
- Reduced lung function, leading to more frequent symptoms
- Weight gain, which puts extra thoracic strain on the lungs and increases fatigue
- Increased risk of infections due to poor circulation and reduced airway clearance
- Decreased overall fitness, making short walks or stairs feel exhausting
Regular low-to-moderate intensity exercise can help:
- Improve lung capacity
- Strengthen respiratory muscles
- Enhance circulation, reduce airway inflammation and sputum plugging
- Improve physical endurance for daily activities
- Boost mental well-being and reduce anxiety about breathlessness
The key is to choose the right exercises, pace yourself, and follow breathing techniques that help control symptoms.
Best Types of Exercise for Chronic Respiratory Conditions
Not all exercises are suitable for people with asthma, bronchiectasis, COPD, or interstitial lung disease. It’s important to select activities that improve lung function, endurance, and overall health without placing excessive strain on your breathing.
Walking
Walking is one of the best low-impact exercises for lung health. It strengthens muscles without overloading the lungs, helps improve endurance and lung capacity, and can be adjusted for pace and intensity.
Start with short, slow-paced walks and gradually increase your exercise duration. If you experience significant breathlessness, stop, rest, and focus on breathing techniques before continuing.
Strength Training
Building muscle strength improves your lung capacity, making breathing easier. Use light weights or resistance bands for arms and legs, bodyweight exercises like seated squats or wall push-ups, and slow, controlled movements to prevent overexertion.
Yoga and Breathing Exercises
Yoga may help improve flexibility, posture, and breathing control. Deep breathing techniques used in yoga have shown in limited studies to help expand lung capacity and strengthen respiratory muscles in patients with chronic lung disease, such as COPD.
Recommended breathing exercises include pursed-lip breathing to slow breathing and prevent breathlessness and diaphragmatic breathing to encourage deep lung expansion and strengthen breathing muscles.
Water-Based Exercise (Swimming or Aqua Aerobics)
Water exercises are gentle on the lungs while providing low-impact, full-body movement. Swimming in warm, humid air may be beneficial for asthma or bronchiectasis as it reduces airway irritation.
Cycling (Stationary or Outdoor)
Cycling can help increase stamina and improve circulation. Stationary bikes provide a controlled environment where you can adjust resistance to match your fitness level.
Pulmonary Rehabilitation
Pulmonary rehabilitation is a structured weekly or twice-weekly group-based community exercise program designed to empower patients with chronic lung conditions manage their breathlessness and improve their quality of life. It has been shown consistently to be effective in improving the morbidity and exercise tolerance of patients with chronic lung disease, such as COPD.
It includes:
- Exercise training: To improve strength and endurance.
- Education: To learn about your condition and how to manage it.
- Nutrition advice: To support your lung health with a healthy diet.
- Breathing techniques: To help you breathe more easily during episodes of acute breathlessness.
- Emotional support: Helping with stress, anxiety, and depression.
- Peer support: Many clients report the emotional support of improving their respiratory symptoms together with others who share similar chronic lung conditions.
This program can help you manage symptoms, improve your ability to do everyday activities, and feel better overall. You can be referred to a local Pulmonary Rehabilitation Program by your GP, Physiotherapist or Respiratory Specialist.

Managing Breathlessness During Exercise
Breathlessness is normal when exercising, but it shouldn’t cause extreme discomfort or force you to stop completely. If you experience excessive breathlessness, follow these techniques.
Pursed-Lip Breathing
This technique slows breathing and helps maintain open airways. Inhale through your nose for two seconds, exhale slowly through pursed lips (as if blowing out a candle) for four seconds, and repeat until breathing normalises.
Controlled Pacing
Move slowly and steadily instead of rushing through activities. Take breaks between sets of exercises or incline changes. Avoid holding your breath during physical effort—exhale during exertion.
Use Your Reliever Inhaler or Short-Acting Medications (if prescribed)
For people with asthma or COPD, using a bronchodilator inhaler (reliever) 10 to 15 minutes before exercise can help reduce symptoms of breathlessness prior to exertion.
For people with advanced or end-stage lung disease, such as COPD or interstitial lung diease, using short-acting opoids or benzodiazepines (such as Ordine or Lorazepam) 10 to 15 minute s before exertion as prescribed by your GP, Palliative Care or Respiratory Physician, can also reduce your overall symptom burden.
Maintain Good Posture
Sitting upright with relaxed shoulders allows the lungs to expand more fully. If you feel breathless, try leaning forward slightly with hands on knees or a surface for support or sitting with arms resting on your thighs to stabilise breathing.
Exercising with Different Respiratory Conditions
Asthma and Exercise
Avoid cold air, dry air, pollen and pollution, as they can trigger symptoms. Warm up before exercise and cool down gradually. If you experience wheezing or tightness, stop and use a reliever inhaler as prescribed.
COPD and Exercise
Exercise in short bursts with rest in between. Avoid overexertion and aim for moderate effort rather than high intensity. Use pursed-lip breathing to control breathlessness.
Bronchiectasis and Exercise
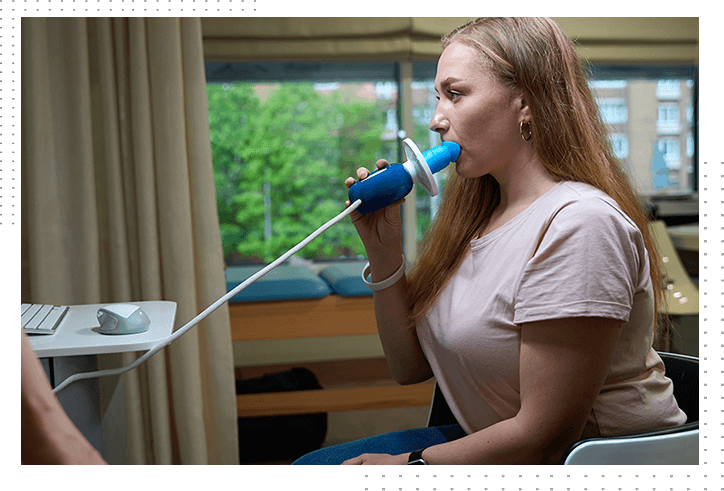
Focus on consistent and regular daily airway clearance with the use of devices, including bubble PEP and Flutter Valve. Keep well hydrated to keep mucus thin and easier to clear. Avoid overly humid environments that can worsen mucus buildup. Optimise your nutrition.
Interstitial Lung Disease (ILD) and Exercise
Use ambulatory oxygen therapy or medications to aid with breathlessness (such as short-acting opioids or benzodiazepines) if prescribed, and pace yourself. Choose gentle movements to prevent extreme fatigue. Work on breath control techniques to improve efficiency.
When to Stop Exercise and Seek Medical Advice
Stop exercising and seek medical advice if you experience severe breathlessness that doesn’t improve with rest, dizziness, chest pain, palpitations, extreme wheezing, or excessive fatigue lasting hours after exercise.
If you are unsure about safe exercise options for your condition, consult your GP, Physiotherapist or local Respiratory Physician to develop a safe, personalised exercise program.

Final Thoughts
Staying physically active is one of the best ways to manage breathlessness and maintain lung function. By choosing the right exercises, pacing yourself, and using breathing techniques, you can improve your fitness and quality of life while living with a chronic lung condition such as asthma, COPD, bronchiectasis, or interstitial lung disease.


